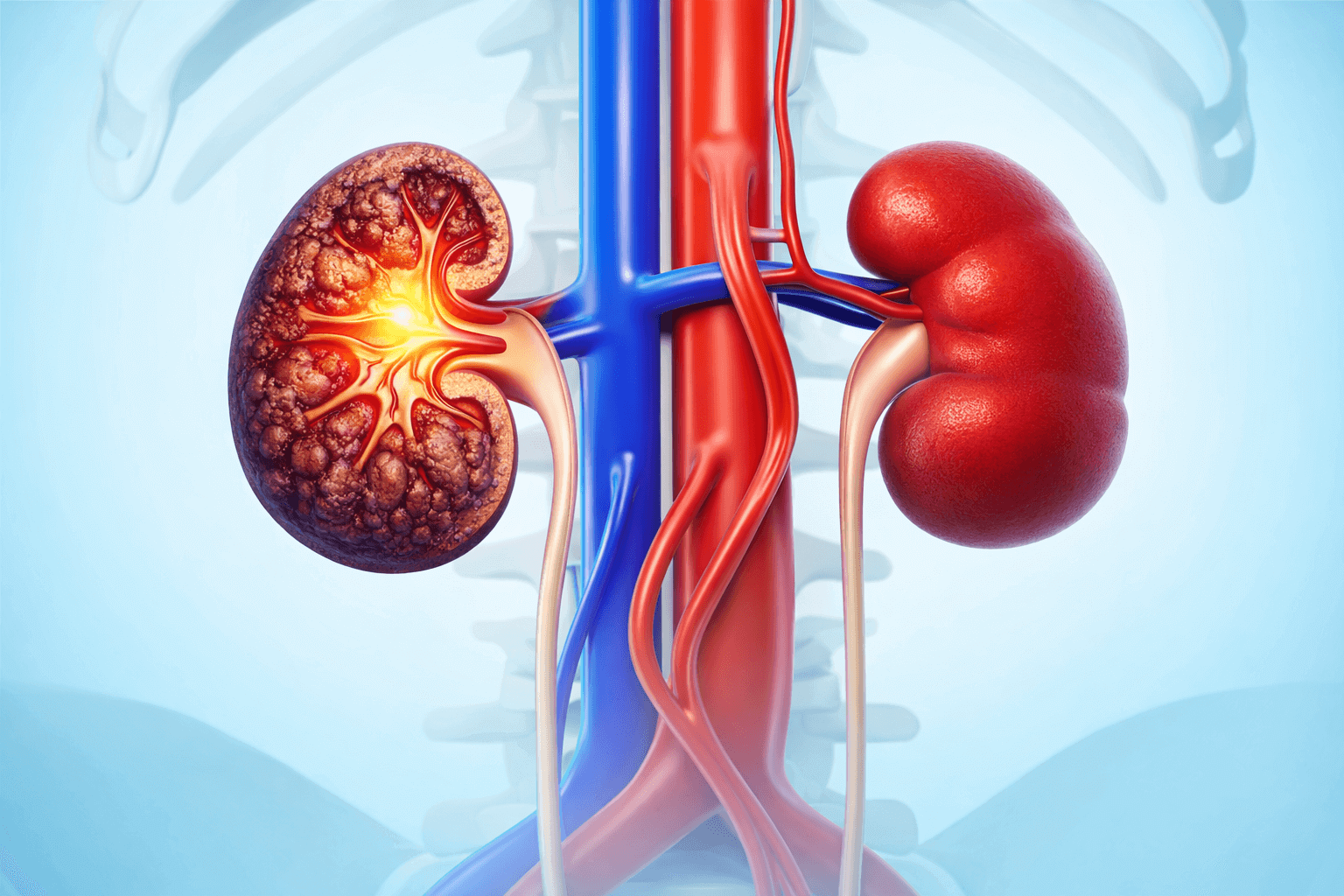
If you were told you have stage 3 kidney disease (also called stage 3 chronic kidney disease or CKD stage 3), you’re not alone—and you’re not “at kidney failure.” Stage 3 means your kidneys are working less efficiently than they should, but many people can stay stable for years with the right plan.
What worries me as an ER doctor isn’t the label itself. It’s when someone doesn’t realize how common CKD is, misses early clues, or ignores warning symptoms that shouldn’t wait.
This article is for education—not a diagnosis. If you’ve been told you have CKD, your primary doctor and/or a nephrologist should guide your long-term plan.

What does stage 3 kidney disease mean?
Doctors stage CKD mainly using eGFR (estimated glomerular filtration rate)—a blood-test estimate of how well your kidneys filter waste.
Stage 3a vs. Stage 3b
Stage 3 is split into two sub-stages:
- Stage 3a CKD: eGFR 45–59 for 3+ months
- Stage 3b CKD: eGFR 30–44 for 3+ months
This split helps clinicians understand risk and how closely to monitor things.
Is stage 3 kidney disease serious?
It’s serious in the sense that it increases your risk for complications and future decline—but it’s also a stage where you can still do a lot to protect your kidneys.
Stage 3 is often when people first find out they have CKD, and symptoms may be mild or absent early on.
CKD stage 3 symptoms: what people actually notice
Many people with stage 3a have no obvious symptoms; symptoms can start to appear as kidney function declines.
When symptoms show up, they often look like “everyday” issues—fatigue, itching, swelling, appetite changes—so they get brushed off.
Possible symptoms in stage 3a
- Changes in urination (more or less than usual)
- Itchy/dry skin
- Feeling tired
- Nausea, decreased appetite
- Unintentional weight loss
Symptoms may become more noticeable in stage 3b
- Urinating more or less than usual
- Itchy/dry skin
- Fatigue, trouble concentrating
- Numbness or swelling in legs/ankles/feet
- Muscle cramps
- Shortness of breath
- Nausea/vomiting, loss of appetite
What causes stage 3 kidney disease?
The most common causes in adults are:
- Diabetes
- High blood pressure (hypertension)
Other causes exist (autoimmune disease, inherited conditions, certain long-term medications, repeated kidney infections, obstruction, etc.), but diabetes and hypertension lead the list.
Can stage 3 kidney disease be reversed?
In most cases, CKD is not “reversed” in the way an infection is cured—because CKD means chronic, long-term damage. The goal is to slow progression and reduce complications, sometimes keeping kidney function stable for a long time.
What matters most is consistent follow-up and controlling the drivers—especially blood pressure and diabetes. NIDDK emphasizes blood pressure control as a key step and outlines practical management steps (BP control, glucose goals, medication adherence, dietitian support, etc.).
What creatinine level is stage 3 kidney disease?
This is a very common question—and it’s a good one.
Here’s the honest answer: there isn’t one single creatinine number that defines stage 3 for everyone. eGFR is calculated using creatinine plus factors like age and sex, so two people can have the same creatinine and different eGFRs.
If you want clarity, ask your clinician:
- “What is my eGFR trend over time?”
- “What is my uACR (urine albumin/creatinine ratio)?”
The two tests that matter most: eGFR + urine albumin (uACR)
To understand CKD risk, clinicians typically look at:
- eGFR (blood test) – kidney filtering estimate
- uACR (urine albumin-to-creatinine ratio) – checks if protein is leaking into urine (a sign of kidney damage)
What uACR results can mean
- A urine albumin result 30 mg/g or higher may mean kidney disease, and tests are often repeated to confirm.
- NKF notes <30 mg/g is considered normal and >30 mg/g may indicate kidney disease (even if eGFR is above 60).
- NIDDK similarly describes uACR above 30 mg/g as higher than normal.
Stage 3 CKD complications (what your doctor may screen for)
Stage 3 is where clinicians start paying closer attention to complications, including:
- Anemia
- Mineral and bone disorder
- Metabolic acidosis
That doesn’t mean you will develop these issues—but it’s why follow-up labs matter.
What you can do to protect your kidneys (practical, not gimmicky)
This is the part I wish more people heard early—because it’s where you can truly add years of stability.
1) Control blood pressure
NIDDK calls blood pressure control the “most important step” for many people with CKD and lists practical strategies (low-sodium meals, activity, sleep, medication adherence).
2) Hit your diabetes targets if you have diabetes
Managing glucose reduces kidney strain and helps protect long-term function.
3) Eat in a kidney-smart way
NIDDK’s CKD nutrition guidance focuses on choosing healthy foods and avoiding foods high in sodium, potassium, and phosphorus when appropriate, because the right plan depends on your labs and stage.
Important: There is no one perfect “CKD diet” for everyone. Your potassium/phosphorus needs depend on lab results and your overall health.
4) Be careful with OTC pain meds
The National Kidney Foundation warns that NSAIDs (like ibuprofen/naproxen) can reduce blood flow to the kidneys and raise risk of kidney damage—especially with higher doses or long-term use.
If you have CKD, always ask your clinician what’s safe for you before using OTC meds regularly.
Warning symptoms that shouldn’t wait (when to go to the ER)
Most CKD care is outpatient. But some symptoms suggest a problem that needs urgent evaluation—especially if you feel significantly worse or symptoms are escalating.
Consider urgent ER evaluation for things like:
- Shortness of breath, especially if worsening or new
- Severe swelling in legs/feet or swelling that’s rapidly getting worse
- Persistent vomiting or inability to keep fluids down
- Marked decrease in urination (or not peeing much at all)
- Confusion, chest pain, fainting, severe weakness (these can overlap with multiple emergencies and shouldn’t be monitored at home)
If you’re unsure, it’s better to be evaluated than to wait and deteriorate.
If you’re in the Post Oak / Galleria area—or nearby neighborhoods like Uptown, Tanglewood, River Oaks, Memorial, or Westchase—and you’re dealing with warning symptoms that shouldn’t wait, Post Oak ER is open 24/7 with board-certified physicians, and on-site diagnostics to evaluate urgent medical concerns.
Post Oak ER is a freestanding emergency facility, and the site notes it provides hospital-grade emergency care in the community.
Frequently Asked Questions
Is stage 3 kidney disease life-threatening?
Not by itself. Many people live for years with stage 3 CKD—especially when the underlying causes (like blood pressure and diabetes) are controlled. The key is trends over time, not one lab value.
What’s the difference between stage 3a and stage 3b kidney disease?
Stage 3a is eGFR 45–59; stage 3b is eGFR 30–44 (for 3+ months).
Do you feel symptoms in stage 3 CKD?
Often no, especially in stage 3a. Symptoms may become more noticeable in stage 3b.
What tests should I ask my doctor about?
At minimum: eGFR and uACR. These help determine kidney function and kidney damage risk.
What does uACR 30 mg/g mean?
A urine albumin result 30 mg/g or higher may indicate kidney disease, and clinicians often repeat tests to confirm.
What foods should I avoid in stage 3 kidney disease?
It depends on labs and your overall health. NIDDK emphasizes that avoiding foods high in sodium, potassium, and phosphorus may help prevent or delay CKD-related problems—when clinically appropriate.
Can I take ibuprofen if I have CKD?
Be cautious. NKF warns NSAIDs can harm kidney blood flow and raise risk of kidney damage—especially with long-term/high-dose use. Talk with your clinician about safer options for your situation.
What’s the #1 thing that helps slow CKD progression?
For many people: blood pressure control and diabetes control, plus regular monitoring and a personalized plan.