Key Takeaways
- Pancreatitis is inflammation of the pancreas and can be acute (sudden) or chronic (long-lasting).
- Abdominal pain—often in the upper abdomen and sometimes radiating to the back—is a primary symptom.
- Severity varies: many acute cases improve within days, while severe cases can be life-threatening.
- Diagnosis and treatment depend on cause and severity and often require medical evaluation.
Overview
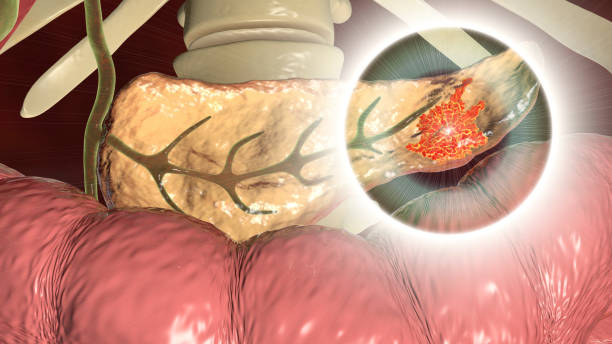
Pancreatitis is inflammation of the pancreas. The pancreas is a gland behind the stomach that helps digestion by making digestive enzymes and helps regulate blood sugar by making hormones such as insulin. Pancreatitis can happen suddenly (acute pancreatitis) or be long-lasting (chronic pancreatitis). Either form can be serious and can lead to complications.
Pancreatic Function
The pancreas has two main functions:
- Digestion: It makes digestive juices (enzymes) that help digest food.
- Blood sugar regulation: It makes hormones such as insulin that help regulate blood sugar.
In pancreatitis, pancreatic enzymes can damage the pancreas and trigger inflammation.
Types of Pancreatitis
Acute Pancreatitis
- Starts suddenly and is usually a short-term condition.
- Many people improve and recover in several days with treatment, though severe cases may require a longer hospital stay and can develop serious complications.
Chronic Pancreatitis
- A long-lasting condition in which the pancreas does not heal or improve and can worsen over time.
- Can lead to lasting damage (including scarring) that interferes with normal pancreatic function, including digestion and blood sugar regulation.
- Some people with chronic pancreatitis have complications before they notice symptoms.
Symptoms
Common Symptoms
Abdominal pain is a primary symptom. Pain may:
- Be in the upper abdomen
- Spread (radiate) to the back
- Feel worse after eating in some cases
Other symptoms that can occur (especially in acute pancreatitis) include:
- Nausea and vomiting
- Fever
- Fast heartbeat
Symptoms More Common in Chronic Pancreatitis
- Upper abdominal pain (some people have no pain)
- Pain that may spread to the back, become constant and severe, and become worse after eating
- Weight loss
- Greasy, foul-smelling stools
- Diarrhea, nausea, vomiting
Causes
Common causes include:
- Gallstones
- Heavy alcohol use
- Some medicines
- Genetic disorders affecting the pancreas
Other causes can include:
- Blockage in the pancreatic duct
- High levels of blood fats (lipids)
- High blood calcium levels
- Infections
- Injury to the abdomen
- ERCP (a procedure used to treat another condition)
Sometimes, doctors can’t identify a cause (idiopathic pancreatitis).
Diagnosis
Clinicians may use:
- Medical history and physical exam
- Lab tests, including blood tests that can measure amylase and lipase
- Stool tests in some situations (for example, to evaluate fat malabsorption)
- Imaging tests such as ultrasound, CT scan, and MRCP, depending on the clinical situation
Treatment
Treatment depends on the cause and severity and may include hospital care to manage symptoms and complications. Supportive treatment can include:
- Intravenous (IV) fluids
- Pain medicines
- Nutrition support (for example, if eating isn’t possible due to symptoms, a feeding tube may be used)
- In some cases, being advised not to eat solid foods for a period
Treating the underlying cause may involve procedures such as ERCP to locate and remove gallstones in appropriate cases.
Possible Complications
- Severe acute pancreatitis can cause a systemic reaction that may lead to shock and multiple organ failure.
- Severe acute pancreatitis can involve necrosis and infection and may become life-threatening.
- Chronic pancreatitis can lead to malabsorption and malnutrition over time.
- Chronic pancreatitis can lead to problems regulating blood sugar and may lead to diabetes.
Recovery and Outlook
- Many people with acute pancreatitis start to feel better within about a week, and many are well enough to leave the hospital after a few days.
- Recovery can take longer in severe cases, especially if complications develop.
- Chronic pancreatitis is a long-term condition that may require ongoing management and follow-up over time.
When to See a Doctor
Seek medical care right away if you have symptoms that could indicate severe pancreatitis, such as:
- Severe or worsening abdominal pain or tenderness
- Nausea and vomiting
- Fever or chills
- Fast heartbeat
- Shortness of breath
- Yellowing of the skin or whites of the eyes (jaundice)
You may not be able to tell how severe pancreatitis is based on symptoms alone, so urgent evaluation is recommended when symptoms are significant.
Frequently Asked Questions
Where is pancreatitis pain located?
Pain is commonly felt in the upper abdomen and may radiate to the back.
Can pancreatitis pain get worse after eating?
Yes. Pain in pancreatitis may feel worse after eating, and in acute pancreatitis, eating may make symptoms feel worse quickly.
Can back pain and stomach pain happen together in pancreatitis?
Yes. Abdominal pain in pancreatitis may spread to the back.
Does pancreatitis cause lower back pain or lower abdominal pain specifically?
There is no high-quality evidence supporting this.
How long does acute pancreatitis last?
Acute pancreatitis often improves within several days with treatment, but more severe cases may require a longer hospital stay.
Can pancreatitis go away on its own?
Some cases of acute pancreatitis may go away on their own, but this depends on what caused it and how severe it is. Medical evaluation is still recommended when symptoms occur.
Is pancreatitis deadly?
Pancreatitis can be serious. Severe acute pancreatitis can lead to life-threatening complications, including organ failure, and may be fatal.
Is dehydration a reason to seek emergency care for pancreatitis?
There is no high-quality evidence supporting this.
Can I see a picture of the pancreas?
There is no high-quality evidence supporting this.
What is pancreatitis?
Pancreatitis is inflammation of the pancreas.
What causes pancreatitis?
Common causes include gallstones and heavy alcohol use, as well as genetic disorders of the pancreas and some medicines. Other causes are possible, and sometimes the cause is unknown.
How is pancreatitis diagnosed?
Diagnosis may include medical history, physical exam, lab testing (including pancreatic enzymes such as amylase and lipase), imaging tests, and sometimes stool tests.
What are common treatments?
Treatment often involves hospital-based supportive care such as IV fluids, pain medicines, and nutrition support when needed, plus treatment of the underlying cause when appropriate.
Is pancreatitis contagious?
There is no high-quality evidence supporting this.
APA Reference List
Cleveland Clinic. (2023, January 12). Pancreatitis. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/8103-pancreatitis
Mayo Clinic Staff. (2025, October 31). Pancreatitis: Diagnosis and treatment. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/pancreatitis/diagnosis-treatment/drc-20360233
Mayo Clinic Staff. (2025, October 31). Pancreatitis: Symptoms and causes. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/pancreatitis/symptoms-causes/syc-20360227
Mayo Clinic Health System. (n.d.). Pancreatitis. Mayo Clinic Health System. https://sncs-prod-external.mayo.edu/locations/sparta/services-and-treatments/gastroenterology-and-hepatology/digestive-disorders/pancreatitis
National Health Service. (2022, May 24). Acute pancreatitis. NHS. https://www.nhs.uk/conditions/acute-pancreatitis/
National Health Service. (2022, May 24). Acute pancreatitis: Complications. NHS. https://www.nhs.uk/conditions/acute-pancreatitis/complications/
National Institute of Diabetes and Digestive and Kidney Diseases. (2017, November). Diagnosis of pancreatitis. National Institutes of Health. https://www.niddk.nih.gov/health-information/digestive-diseases/pancreatitis/diagnosis
National Institute of Diabetes and Digestive and Kidney Diseases. (2017, November). Pancreatitis. National Institutes of Health. https://www.niddk.nih.gov/health-information/digestive-diseases/pancreatitis
National Library of Medicine. (2024, September 13). Pancreatitis. MedlinePlus. https://medlineplus.gov/pancreatitis.html
NHS inform. (2025, July 9). Acute pancreatitis. NHS inform. https://www.nhsinform.scot/illnesses-and-conditions/stomach-liver-and-gastrointestinal-tract/acute-pancreatitis/