If you or someone you love has been told “you may need dialysis,” it can feel like the ground shifts under your feet. Dialysis is a treatment that does part of the work your kidneys can’t do anymore—filtering waste and extra fluid—when kidney failure is advanced.
CDC notes that more than 1 in 7 U.S. adults may have chronic kidney disease (CKD), and as many as 9 in 10 don’t know they have it.
For some people, CKD progresses to kidney failure—where dialysis or transplant becomes necessary to survive.
Educational only. Not a diagnosis or personal medical advice.
What is dialysis, in plain English?
Dialysis is a medical treatment that helps your body by:
- removing waste products your kidneys normally filter out
- removing extra fluid that can build up in the body
- helping maintain a safer balance of minerals and electrolytes
Does dialysis cure kidney failure?
No—dialysis is not a cure, but it can help you feel better and live longer.
NIDDK also explains that none of the kidney failure treatment options (dialysis, transplant, or conservative management) make the kidneys “get better,” but they can help you feel better.
Who needs dialysis (and when does it happen)?
Dialysis is used for kidney failure (often called end-stage kidney disease).
Many people live for years with earlier-stage CKD (like Stage 3 or Stage 4) without dialysis. Dialysis becomes part of the conversation when kidney function is severely reduced and symptoms, labs, or fluid/electrolyte issues indicate the body needs help.
The main types of dialysis
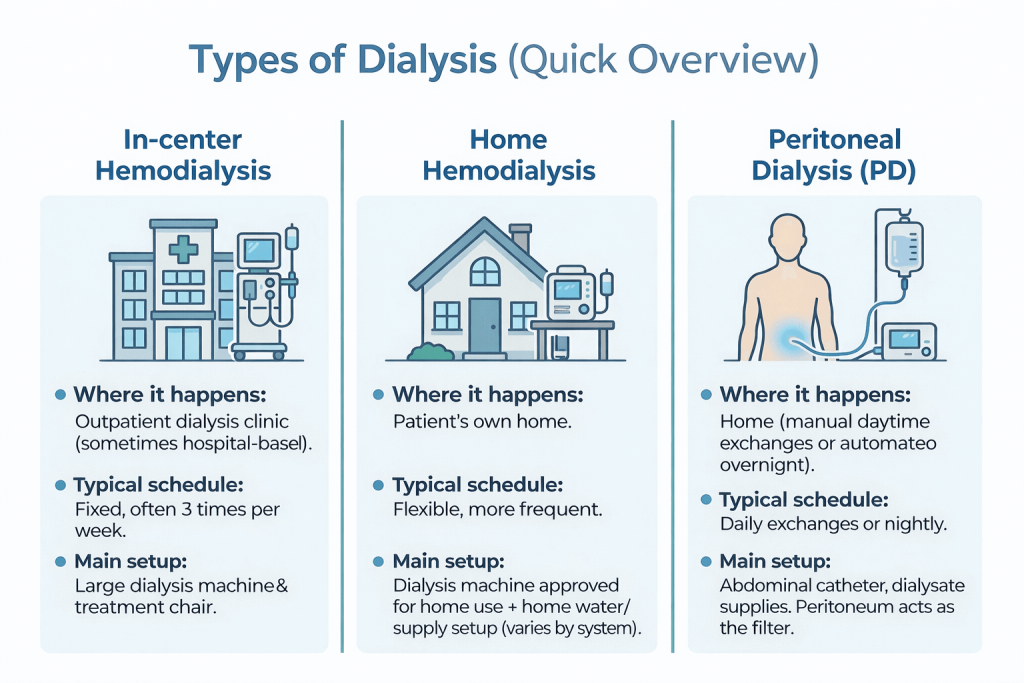
National Kidney Foundation explains there are three main dialysis categories:
- In-center hemodialysis
- Home hemodialysis
- Peritoneal dialysis
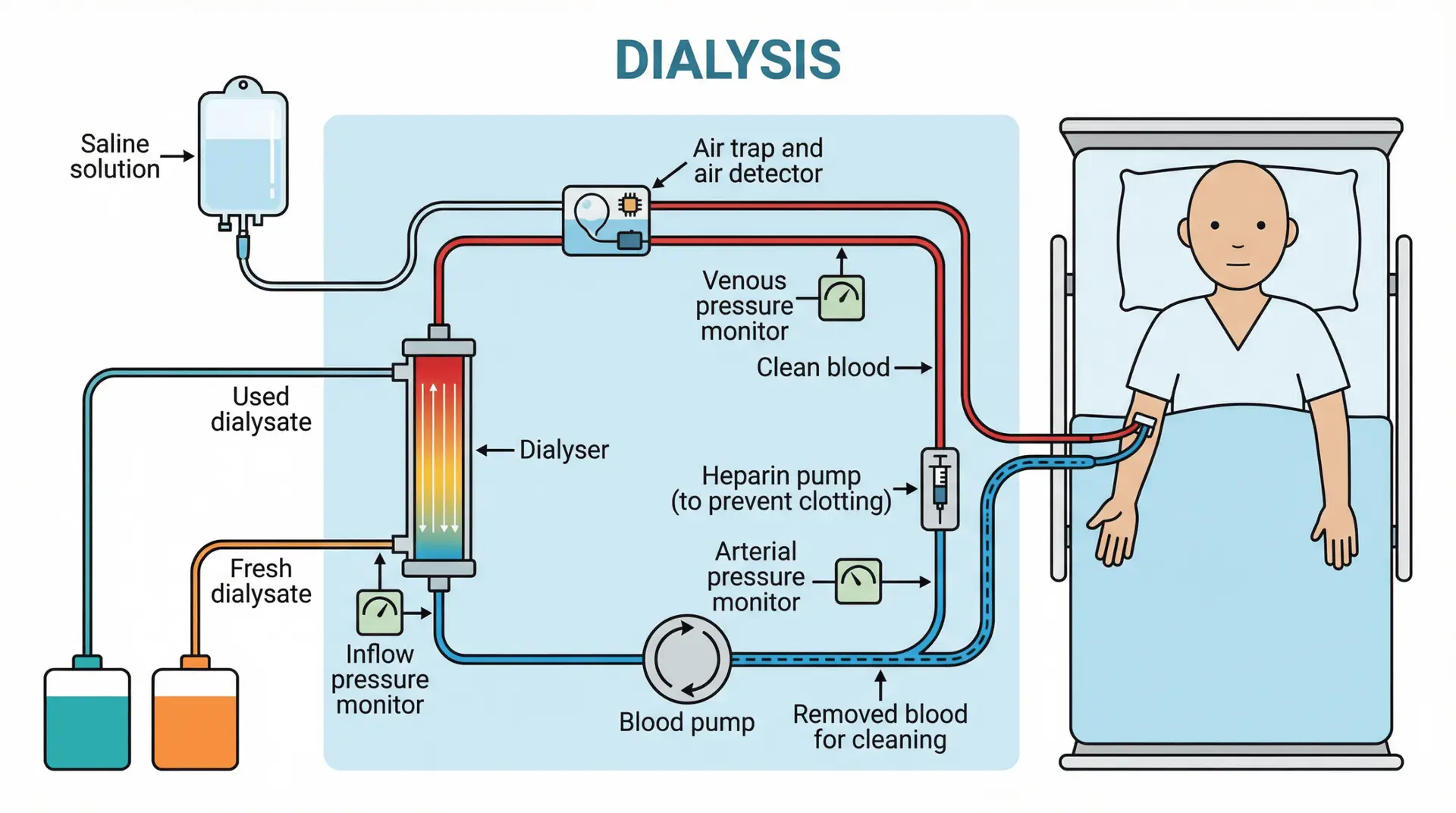
Hemodialysis (blood is filtered outside the body)
NIDDK explains that during hemodialysis, blood goes through a filter (dialyzer) outside the body.
NKF describes hemodialysis as a life-saving treatment that removes waste/extra fluid and helps regulate blood pressure.
Access matters: Before regular hemodialysis, most patients need a vascular access (often a fistula or graft), and NIDDK calls that access your “lifeline.”
Peritoneal dialysis (PD) (filtering happens inside the body)
NIDDK explains PD uses the lining of the abdomen (the peritoneum) to filter blood inside the body, using dialysis solution that flows in and out through a catheter.
Types of PD (NIDDK):
- CAPD (manual exchanges during the day)
- Automated peritoneal dialysis (cycler machine while you sleep)
A practical scheduling detail: NIDDK notes CAPD exchanges typically take 30–40 minutes, dwell time is often 4–6 hours or more, and people usually do exchanges at least four times a day.
NIDDK also notes automated PD can do exchanges three to five times during the night with a cycler.
Where PD can be done: NIDDK states PD can be done in clean private places—including home, work, or while traveling (with planning for supplies).
How common is PD? Cleveland Clinic notes peritoneal dialysis is the least common dialysis type and estimates about 10% of people who need dialysis receive PD.
How do people choose the “right” dialysis?
This is a personal decision—and it’s normal to revisit it.
National Kidney Foundation emphasizes that each dialysis type has pros/cons and you can often change modalities over time, so you don’t have to feel “locked in.”
NIDDK also encourages learning about options early and working with your care team to build a plan before dialysis is urgently needed.
In real life, the choice often comes down to:
- your overall health and other conditions
- your home setup/support
- your work/life schedule
- whether home therapy is realistic and safe
- what your nephrology team recommends
Common dialysis questions
“Does dialysis hurt?”
Most people don’t describe dialysis itself as “painful,” but it can be uncomfortable—especially early on—because it’s a major change for your body and routine. NIDDK notes adjusting to dialysis and kidney failure can be hard, and diet/fluid changes may be needed.
“What side effects can happen?” (hemodialysis)
NIDDK lists possible issues like:
- muscle cramps
- a sudden drop in blood pressure (hypotension), which can cause weakness, dizziness, or nausea
“Why do dialysis patients have fluid limits?”
NIDDK explains fluid can build up in the body between hemodialysis treatments, and many patients need to limit sodium and fluids.
“Can I travel while on dialysis?”
NIDDK notes PD can be done while traveling with planning (including shipping supplies to where you’re going).
For hemodialysis, travel is possible but typically requires scheduling treatments at a dialysis center at your destination (your dialysis team helps coordinate).
Warning symptoms that shouldn’t wait
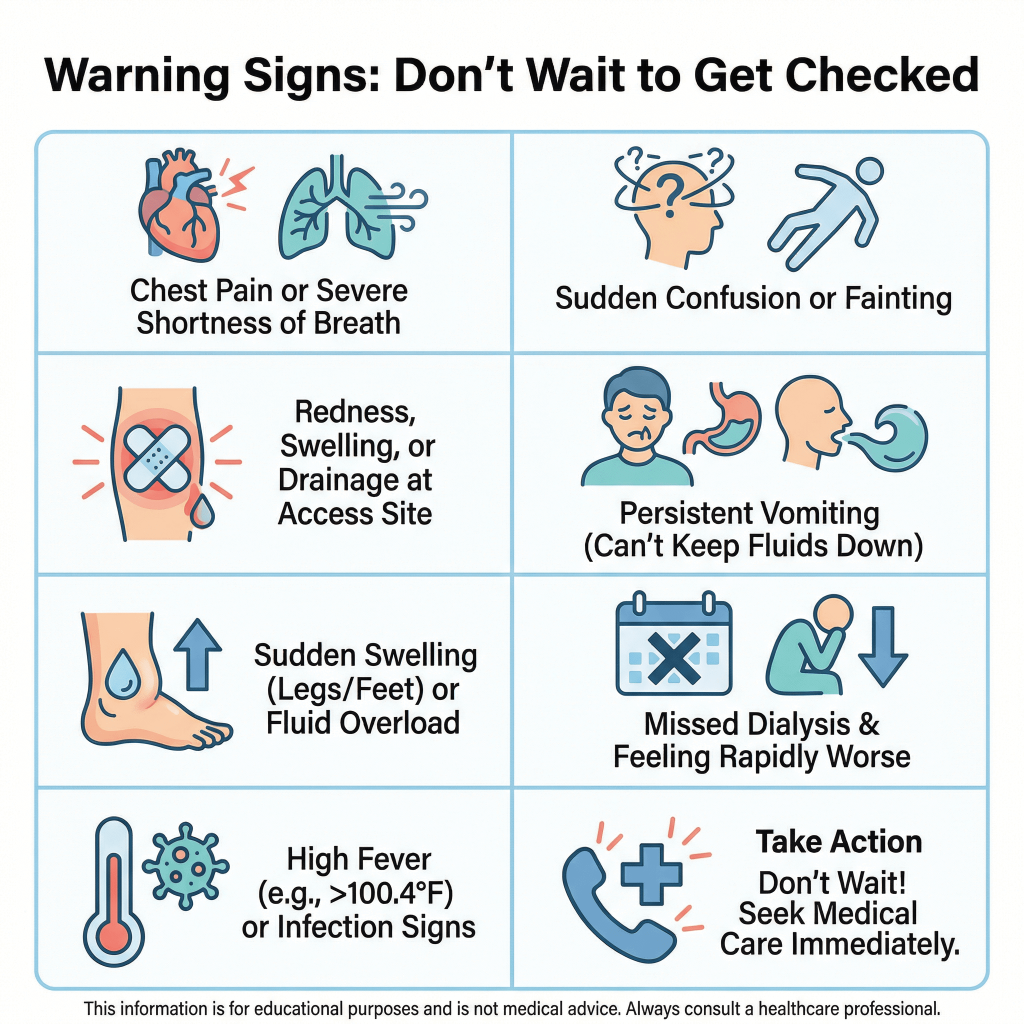
Dialysis patients can get sick quickly when something is “off.” Consider urgent evaluation if you have any of the following:
- Chest pain, severe shortness of breath, fainting, or confusion (these are emergency-level symptoms regardless of kidney history)
- Signs of infection at your dialysis access (warmth, redness, drainage, worsening pain). NIDDK specifically advises checking access sites for warmth/redness and notifying your center if you can’t feel the vibration over the access.
- Persistent vomiting or inability to keep fluids down (risk of dehydration and dangerous electrolyte shifts)
- Sudden, significant swelling or worsening shortness of breath (can suggest fluid overload)
- You missed dialysis and feel rapidly worse (severe weakness, shortness of breath, chest discomfort, severe nausea)
If you’re ever uncertain, it is safer to be evaluated than to wait.
If you’re in Houston—especially near Uptown, the Galleria area, the Energy Corridor, Westchase, Midtown, or the Heights—and you’re dealing with warning symptoms that shouldn’t wait, getting checked promptly is reasonable.
Post Oak ER states it is open 24/7 and located right off San Felipe St. near The Galleria and Uptown Park, making it accessible from multiple Houston areas.
They also state they have on-site lab testing and imaging (CT, X-ray, ultrasound) available.